Abstract
Drug-induced liver injury (DILI) has been the biggest single cause of safety-related drug withdrawals for the past 50 years. DILI-related events after drug approvals have led to box warnings restricting the marketability of many drugs and reminding patients that even the most promising medications can have unintended consequences. Solving a puzzle in its myriad forms requires decoding the code. As science and technology move forward, DILI is being seen through a new lens—one that promises not only a better understanding, but also innovative solutions. Entangled in metabolic responses, immune responses and genetic variations, DILI is being meticulously dissected through advanced technologies from metabolomics, proteomics, and genomics to microphysiological systems and AI. This immersive webinar presents an innovative trifecta comprising a 3D microphysiological system, assays that scan through cellular vulnerabilities, and highlights how a decision-making algorithm can be used to reduce liver liabilities and potentially exclude patient populations at risk.
Highlights
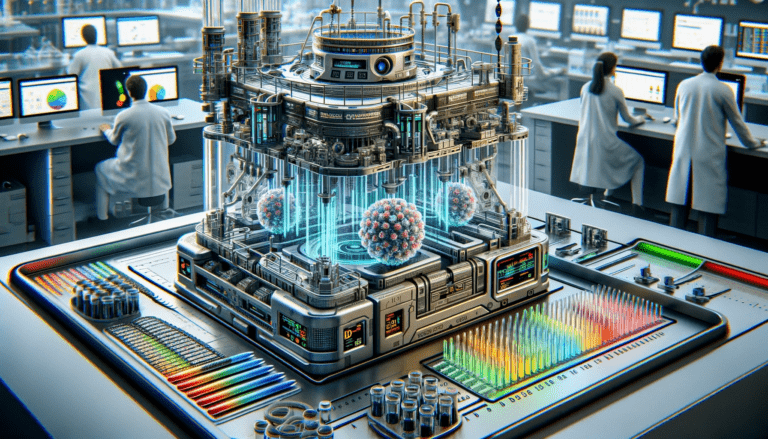
- Perfused Organ Panel microphysiological system with synthetic hemoglobin brings cellular oxidative metabolism, drug metabolism, and mitochondrial utilization closer to physiological levels that are required for drug activity and reactions to the drug.
- Proprietary assays panels then scan through cellular vulnerabilities to find the trigger, a toxicity mechanism which inhibits a specific cellular function at the lowest dose. The trigger sheds light on the cause of toxicity, which may be important in early drug de-risking to understand the relevance of the signal for the intended indication and patient population.
- The assay panels then examine the effects along the dose response curve, specifying which other toxicity mechanisms become active as the dose is increased. Once a signal has been detected during preclinical or clinical development, this information can provide an insight into the origin and/or the mechanism for a specific dose.
Speaker: Dr. James T. Shoemaker, PhD
Chief Science Officer Lena Biosciences
Dr. James T. Shoemaker has been at the forefront of 3D tissue engineering for the past 20 years. As a biomedical engineer and chemist by training, he held appointments at the Emory University and the Georgia Institute of Technology where he developed advanced tissue models for traumatic brain injury and Alzheimer’s disease research.
In 2016, he co-founded Lena Biosciences where he co-developed and validated Perfused Organ Panel platform, the first in vitro platform with synthetic hemoglobin, Blood Substitute, for biomedical research and drug testing.
Lena Biosciences’ scaffold and the platform have since been featured in numerous publications. Faced with the expense of “trapping” DILI, he and the team at Lena Biosciences turned to the pillars of screening and developed their own assays to identify the cause. They are now embarking on establishing a decision-making tree to help drug researchers develop safer drugs, and are sharing their story.